11.1.1 Describe the process of blood clotting
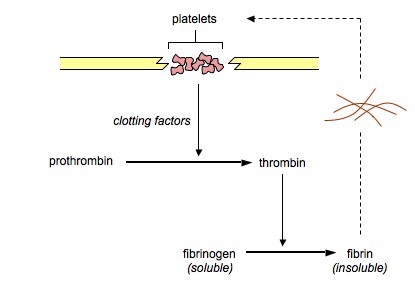
- Clotting (haemostasis) is a mechanism that prevents the loss of blood from broken vessels
- Damaged cells and platelets release chemical signals called clotting factors which trigger a coagulation cascade:
- Clotting factors convert the inactive zymogen prothrombin into the activated enzyme thrombin
- Thrombin catalyses the conversion of the soluble plasma protein fibrinogen into an insoluble form (fibrin)
- Fibrin forms an insoluble mesh of fibres that trap blood cells at the site of damage
- Clotting factors also cause platelets to become sticky, which then adhere to the damaged region to form a solid plug called a clot
- The clot prevents further blood loss and blocks entry to foreign pathogens
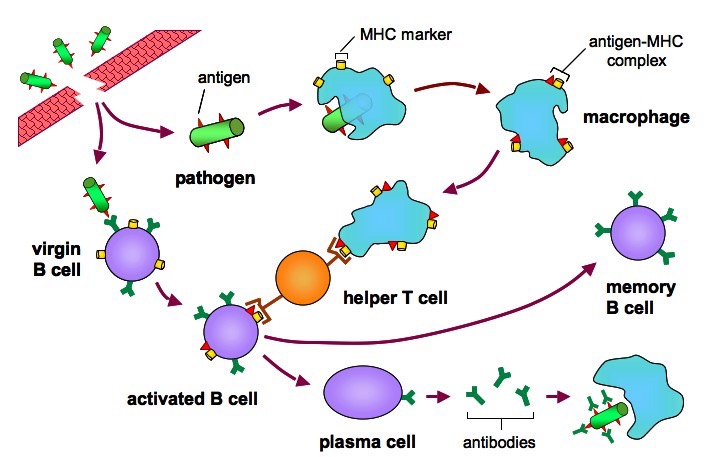
11.1.2 Outline the principle of challenge and response, clonal selection and memory cells as the basis of immunity
Challenge and Response
- When the body is challenged by a foreign pathogen it will respond with both a non-specific and specific immune reaction
- The body is capable of recognising invaders as they do not possess the molecular markers that designated all body cells as 'self' (MHC class I)
- Non-specific immune cells (macrophages) present the foreign antigens to lymphocytes as examples of 'non-self' (on MHC class II)
- These lymphocytes can then respond with the production of antibodies to destroy the foreign invaders
Clonal Selection
- Each B lymphocyte has a specific antibody on its surface that is capable of recognising a specific antigen
- When antigens are presented to B cells (and TH cells) by macrophages, only the B cell with the appropriate antibody will become activated and clone
- The majority of B cell clones will differentiate into antibody-producing plasma cells, a minority will become memory B cells (BM cells)
- Because pathogens may contain several antigenic determinants, several B cell clones may become activated (polyclonal activation)
Clonal Selection

Memory Cells

- Because the adaptive immune response is dependent on clonal expansion to create sufficiently large amounts of antibodies, there is a delay between initial exposure and the production of antibodies
- When a B cell does divide and differentiate into antibody-secreting plasma cells, a small proportion of clones will differentiate into memory cells
- Memory cells remain in the body for years (or even a lifetime)
- If a second infection with the same antigen occurs, the memory cells react faster and more vigorously than the initial immune response, such that the symptoms of the infection do not normally appear
- Because the individual no longer presents with the symptoms of infection upon exposure, the individual is thus said to be immune
11.1.3 Define active and passive immunity
Active immunity: Immunity due to the production of antibodies by the organism itself after the body's defence mechanisms are stimulated by antigens
Passive immunity: Immunity due to the acquisition of antibodies from another organism in which active immunity has been stimulated
- This passive acquisition of antibodies can be achieved via the placenta, colostrum or by injection (e.g. blood transfusions)
11.1.4 Explain antibody production
- Antigens stimulate an immune response via the production of antibodies
- When a pathogen invades the body, it is engulfed by wandering macrophages which present the antigenic fragments on its surface
- This macrophage becomes an antigen-presenting cell, and presents the antigen to helper T cells (TH cells)
- The TH cells bind to the antigen and become activated, and in turn activate the B cell with the specific antibody for the antigen
- This B cell clones and differentiates into plasma cells and memory cells
- The plasma cells produce high quantities of specific antibody to the antigen, whereas memory cells survive in the bloodstream for years
- Upon re-exposure to the antigen, memory cells initiate a faster and stronger response and thus confer long-term immunity
Antibody Production
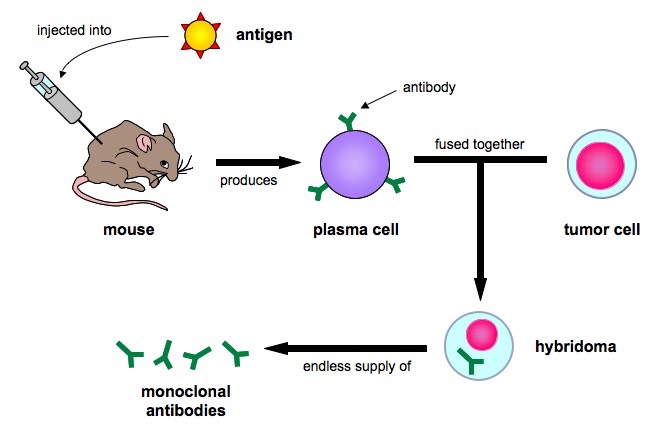
11.1.5 Describe the production of monoclonal antibodies and their use in diagnosis and treatment
- Monoclonal antibodies (mAb) are antibodies derived from a single B cell clone
- An animal (typically a mouse) is injected with an antigen and produces specific plasma cells
- The plasma cells are removed and fused (hybridised) with tumor cells capable of endless divisions (immortal cell line)
- The resulting hybridoma is capable of synthesising large quantities of specific antigen, for use in diagnosis and treatment
Production of Monoclonal Antibodies
Diagnostic Use:
- Monoclonal antibodies can be used to test for pregnancy via the presence of human chorionic gonadotrophin (hCG)
- An antibody specific to hCG is made and is tagged to an indicator molecule (e.g. chromatophore or pigment molecule)
- When hCG is present in the urine it binds to the anti-hCG monoclonal antibody and this complex will move with the fluid until it reaches a second group of fixed antibodies
- When the complex binds to the fixed antibodies, they will appear as a blue line (positive result) due to the presence of the indicator molecule
Treatment Use:
- Monoclonal antibodies can be used for the emergency treatment of rabies
- Because the rabies virus is potentially fatal in non-vaccinated individuals, injecting purified quantities of antibody is an effective emergency treatment for a very serious viral infection
11.1.6 Explain the principle of vaccination
- Vaccinations induce artificial active immunity by stimulating the production of memory cells
- A vaccine contains weakened or attenuated forms of the pathogen and is (usually) injected into the bloodstream
- Because a modified form of the pathogen is injected, the individual should not develop disease symptoms
- The body responds to the vaccine by initiating a primary immune response, resulting in the production of memory cells
- When exposed to the actual pathogen, the memory cells trigger a secondary immune response that is much faster and stronger
- Vaccines confer long-term immunity, however because memory cells may not survive a life time, booster shots may be required
11.1.7 Discuss the benefits and dangers of vaccination
Benefits:
- Vaccination results in active immunity
- It can limit the spread of infectious diseases (pandemics / epidemics)
- Diseases may be eradicated entirely (e.g. smallpox)
- Vaccination programs may reduce the mortality rate of a disease as well as protect vulnerable groups (e.g. youth, elderly)
- Vaccinations will decrease the crippling effects of certain diseases (e.g. polio)
- It will decrease health care costs associated with treating disease conditions
Risks:
- Vaccinated individuals may produce (mild) symptoms of the disease
- There may be human error in the preparation, storage or administration of the vaccine
- Individuals may react badly to vaccines (e.g. hypersensitive / allergic reactions)
- Immunity may not be life long - booster shots may be required
- There may be possible toxic effects of mercury-based preservatives used in vaccines